Latest Version
4.3.18
February 08, 2025
Interactive Communications International, Inc.
Finance
Android
3
Free
com.incomm.otc
Report a Problem
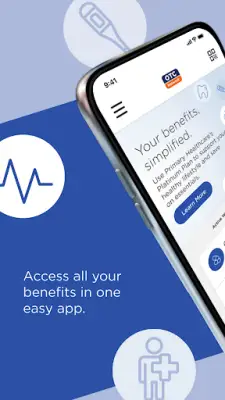
More About OTC Network
The OTC Network app is designed to assist users in effectively tracking and managing their health plan benefits, providing a comprehensive platform for all matters related to their benefits card. With this application, users can easily log in or create an account that connects directly to their particular health plan. This streamlined process ensures that users have direct access to the benefits that are specific to their needs.
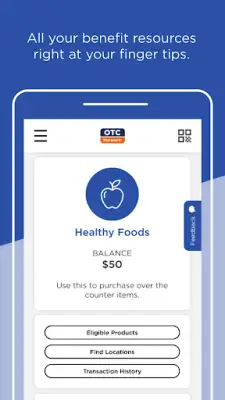
Once users are logged in, they can navigate the app's dashboard, which presents a quick and user-friendly overview of their current benefits and available account balances. This feature allows for easy monitoring of health benefits, ensuring that users are aware of their resources at all times. Each benefit displayed can be clicked on for further details as well as to find related quick actions, making the app not just a tracking tool but a facilitator for managing health benefits efficiently.
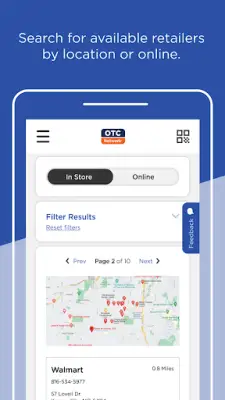
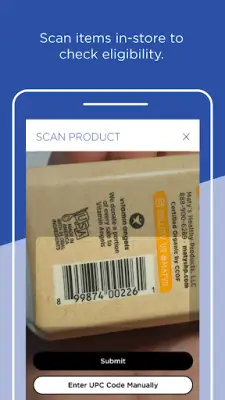
In addition to monitoring balances, the OTC Network app offers various functionalities to enhance the user experience. Users can check their available balances, review transaction history, and search for eligible items that can be purchased. The app also supports online shopping, assists in locating nearby retailers, and includes options for scanning products and making payments directly through the app. These features are designed to maximize convenience while managing health plan benefits.
It is important to note that each user’s health plan comes with a unique set of benefits tailored to fit the specific preferences of their individual members. This variety is made possible by the diverse solutions provided through the OTC Network in collaboration with InComm Healthcare. To understand more about the benefits available and the functionalities of the app, users are encouraged to visit MyBenefitsCenter.com for additional information.
Rate the App
User Reviews
Popular Apps