Latest Version
8.0
April 18, 2025
Aetna Inc
Medical
Android
1
Free
com.aetna.aetnabetterhealthmobile
Report a Problem
More About Aetna Better Health - Medicaid
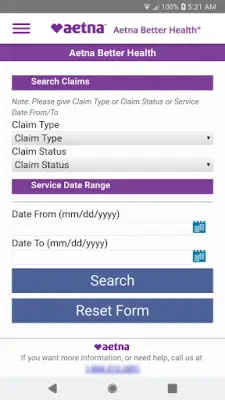
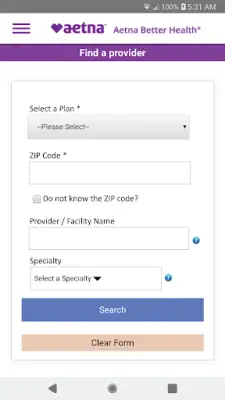
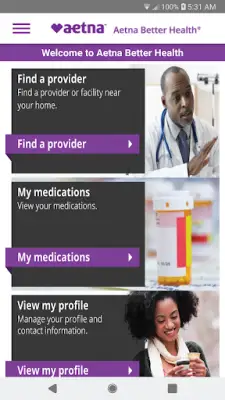
The Aetna Better Health Medicaid application serves as a convenient tool for members to manage their healthcare needs directly from their mobile devices. With this app, users can effortlessly find or change their healthcare providers, ensuring they receive the best possible care tailored to their needs. Additionally, members have the ability to view their medical and prescription claims, making it easier to track their healthcare expenses and stay informed about their treatment history.
Another essential feature of the app is that it allows users to check their current medications. This feature helps members keep track of their prescriptions and manage their medication schedules effectively. Furthermore, users can view their benefits directly through the application, giving them a clear understanding of what is covered under their plan. For new members, the app also offers the option to set up an account that can be accessed through both mobile and web platforms, providing flexibility in how they manage their healthcare information.
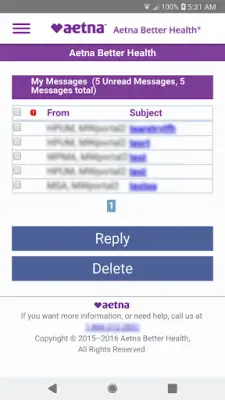
The app fosters communication between members and their health plan through a secure inbox. This feature lets users request various services, such as obtaining an ID card or changing their primary care physician (PCP). By providing a direct line of communication, the app enhances member engagement and ensures that users can easily manage changes in their healthcare needs without added hassle.
Importantly, it is worth noting that Aetna commercial members have access to a different application, the Aetna Mobile App, which they can download to find information relevant to their health plans or search for in-network doctors. The distinct offerings for Medicaid and commercial members highlight Aetna's commitment to providing tailored healthcare solutions that meet the diverse needs of its members.
Rate the App
User Reviews
Popular Apps